Anatomy of the hip
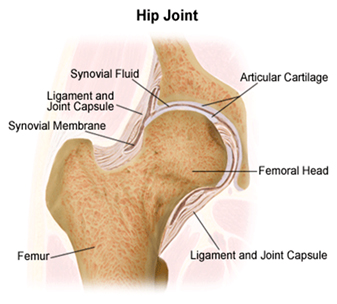
The hip is structurally complex. It is made of bone, ligaments, soft tissue cartlige and muscle. The hip acts as a ball and socket joint. The femur thighbone) has a ball at the end of it which is called the head of the femur.
The socket forms part of the pelvis known as the acetabulum. For the hip to function well, a ball and socket joint is supported by a large muscle mass know as gluteal muscle. Ligaments provide stability for the joint. Soft tissues, nerves and blood vessels provide the hip with nourishment, sensation and protection. The bones that comprise the joint are surrounded with a thin lining of cartilage. This cartilage is known as articulating cartilage, (cartilage that surrounds the bony surface). Articulating cartilage acts as shock absorber and enables the joint to move smoothly in its range of movement.
Osteoarthritis remains the most common cause of hip joint degeneration. The word arthritis literally means joint inflammation (arth “joint”, itis “inflammation”). There are several forms of arthritis. Osteoarthritis is the most common form, and the hip is one of the commonly affected joints. Osteoarthritis especially affects the cartilage in the joint. It is a degenerative process, which directly results in the wearing out of cartilage on the joint surface. Over time, the joint surface slowly erodes, until the underlying bone is exposed. As a result the joint is painful when it moves and bears weight.
Rheumatoid arthritis is a disease of the tissue (synovium), which lines the inside of the joint. Synovium normally produces a slippery fluid, which lubricates the joints. In rheumatoid arthritis, the synovial lining is abnormal. It becomes thicker and secretes abnormally large amounts of poor quality joint fluid which also contains destructive enzymes that dissolve bone, cartilage and tendons. This results in a joint which is inflamed (hot, swollen and painful), stiff and deformed. The initiating cause is unknown, but is thought to be an allergic reaction against the body’s own defences.
Avascular necrosis (AVN) is another form of hip joint degeneration. There is cellular death (necrosis) of bone components due to an interruption in the blood supply. Without blood, the bone tissue dies causing tiny breaks leading to an eventual collapse. Avascular necrosis of bone is often attributed to long-term use of high-dose steroid medications and excessive alcohol intake.
Abnormalities and trauma to the hip joint can also be a cause of joint degeneration. Developmental abnormalities and trauma to the hip joint can be a cause of joint degeneration. Historically, arthritic pain is dull and annoying and primarily in the groin region. It can spread to the thigh and knee. It hurts when you are standing and may improve when you are not taking weight on the hip.
Groin pain with walking
Reduced range of motion
Muscle Stiffness
Difficulty sleeping/night pain
To diagnose degeneration in the hip joint a complete history followed by physical examination is required. Your history is compiled by asking questions about your hip pain, medications you may be taking, and prior injury and other bone and joint problems you may have.A physical examination will assess the range of motion in your hip. Observing how you walk, sit, bend and move will also assist in your assessment.
Further testing may be required if the diagnosis is not clear.
X-ray; this needs to be weight bearing. The use of a weight-bearing x-ray can determine the extent of the degeneration in the joint.
Blood Test; this may determine if there is inflammatory arthritis or infection in the hip.
Scanning and MRI; this can determine if you have avascular necrosis.
Bone Mineral Density; this test determines the condition of the bone or the presence of osteoporosis.
- Hip impingement: A disorder caused by lack of room between the head and neck of femur and the labrum. When the hip is flexed (e.g. in running, sitting, bending), the femur and the labrum rub together which causes pain in the joint.
- Loose bodies: Pieces of bone or cartilage are loose in the joint, often as a result of trauma, injury, or degeneration. This can cause pain, locking and ‘catching’.
- Labral tears: A torn labrum can result either from injury, or from a process of degeneration. It can cause pain, locking or ‘catching’ in the joint.
- Damaged articular cartilage: When cartilage is damaged, torn fragments may protrude into the joint causing pain in when the hip is flexed. The bone under the damaged cartilage no longer has protection from joint rubbing and may eventually become arthritic as a result.
- Femoroacetabular impingement: Excess bone formation on the femoral head or acetabulum. This can restrict movement and cause pain.
- Synovitis: The synovium becomes inflamed and painful.
- Arthritis: Damage to a large amount of articular cartilage.
- Undiagnosed hip pain: Occasionally, hip pain can be present, the cause of which has defied all diagnostic tests to identify.
- Dysplasia of the Hip: Developmental dysplasia (dislocation) of the hip (DDH) is an abnormal formation of the hip in which the femur is not held firmly in the socket. In some cases, the ligaments of the hip joint may be loose and stretched. Also know as clicky hips or dislocating hips.
- Perthes’ Disease: is a disorder of the hip joint in children. The disease has several phases: Initially, there is a temporary loss of blood supply to the femoral head. The lost blood supply causes the ball to soften and collapse. This collapse causes the round femoral head to become flattened or deformed like a mushroom & it no longer fits perfectly in its socket.
Osteoarthritis is a progressive degenerative disease so it has a number of different stages and therefore a number of short and long term treatments.Short term, osteoarthritis can be treated conservatively by diet, exercise modification, medications and physiotherapy.
Long term, however, requires surgical intervention ranging from Arthroscopic Surgery, Hip Resurfacing Surgery & Total Hip Replacement Surgery.
If it has been determined that you require surgery to your hip Professor Kohan and his staff will give you education and guidance to help you prepare.
Various tests will be ordered depending on your medical history.
You should maintain your normal activities of daily living or regular exercise patterns to maintain movement and muscle tone.
It is also important to decrease alcohol intake and if possible, quit smoking.
Preparing your home
- Remove all rugs, loose carpets, obstacles, etc, which may be a hazard on returning home.
- Have available some extra pillows to sleep comfortably at night.
- Bathing in showering accessories may be required, such as a handheld shower.
- Provide easy access to telephone, computer, refrigerator.
- Prepare and refrigerate food before surgery, for easy access in the early postoperative period.
Hospital trip preparation
Prepare personal items to take hospital with you:
- Personal care and hygiene items
- Comfortable walking shoes
- Loose comfortable clothing
- A small amount of money
- Some reading material
- Telephone numbers of persons that may need to be contacted
- Leave valuable jewellery at home
- A list of all medications, supplements, herbs, vitamins ,etc
It is particularity important to remember to advise Professor Kohan & Dr Kerr of the various medications that you are on and then based on their medical evaluation:
Stop taking:
- 3 weeks before your surgery : Your non-steroidal anti-inflammatory (NSAID) medications such as Aspirin, Brufen, Naprosyn, Voltaren, Feldene, etc.
- 3 weeks before your surgery :Holistic and herbal medicines particularly Ginkgo and St John’s wart which may cause excessive bleeding.
Make the following appointments:
-
-
- 1 – 2 weeks prior to Surgery – Anaesthetic consult with Dr Dennis Kerr.
- 7 days post-operation – Appointment in the rooms to check the skin cut.
- 14 days post-operation – Appointment in the rooms to remove skin clips and have an ultrasound to check for a possible blood clot.
- 6 weeks post-operation – Appointment with Professor Kohan for follow-up with an X-ray.
-
Ensure the following tests have been done:
-
-
- Weight bearing X-ray.(No older than 3 months).
- Pathology (full blood count)
- Cross match Blood Test; completed a few days before surgery. This is designed to prepare blood for availability at the time of surgery.
- Chest X-ray
- ECG
-
Complete & return the following Paperwork:
-
-
- Hospital Admission Forms
- Consent Forms – signed & dated
- Estimate of Consult & Surgical Fees – signed & dated
- Estimate of Anesthetist Fees – signed & dated
- Refferal from your GP
- Ensure you have checked with your health fund about covering costs.
- Inform our office about any other health conditions. (For example, heart disease)
-
On the day of surgery:
On the day of surgery you will be expected to arrive at the hospital 2–3 hours prior to your scheduled surgery time ( if you are not admitted the night before). Call the hospital the day before your scheduled surgery date for your expected arrival time.
The operation start time is an estimate, it can be adjusted for various reasons and the staff will inform you if the time has been changed.
Once admitted, the physiotherapist will come and see you to measure you for crutches, walking frame or a cane. The physiotherapist will also provide you with education on how to use these aids.
We recommend that you wear loose fitting slacks (or shorts in the warmer weather) to the hospital. It is much easier for you after surgery. Your family is welcome to visit and stay with you prior to surgery.
When it is time for your surgery, a nurse will assist you to move to the surgical area. Once you arrive in the operating suite you will be taken to an anaesthetic bay where Dr Kerr and his anaesthetic nurse will greet you. When everything is ready, you will be taken into the operating room. The operating rooms must remain cold but extra blankets will be available for you.
- Fasting: Four hours prior to your surgery drink a glass of water. After this point do not eat or drink anything, i.e. do not eat or drink anything 4 hours prior to surgery.
- Pre-operative washing: We advise that in preparation for surgery you shower or bathe using antibacterial Phisohex emulsion. This can be used instead of soap and if used for a week or so before the operation will decrease the population of germs on the skin and by doing so, hopefully decrease the risk of infection. Phisohex can be obtained at the pharmacist and or supermarket. The day before surgery remove nail polish and makeup, if applicable.
- Your Surgical Experience: Immediately after surgery you will wake up in the recovery room. You may feel a bit groggy. Professor Kohan and his staff will monitor you, checking your blood pressure, temperature and pulse. Dr Kerr will also assess your pain level. Post-operative x-rays will be performed in recovery. After 45 minutes – 1 hour you will then be transferred back to your room on the ward.
The prosthetic implant used in hip replacement procedures consist of different parts; the acetabular component, the femoral component and the articular interface. Options exist for different patients and indications. Correct selection of the prosthesis is important.
- Acetabular Component: The Acetabular cup is the component which is placed into the acetabulum (hip socket). Cartilage and bone are removed from the acetabulum and the acetabular cup is attached using friction or cement. Like a healthy hip, your prosthesis has smooth gliding surfaces that allow you to move easily and without pain. Materials may vary, including steel, plastic (Polyethylene) or ceramic. Some acetabular cups are one piece, while others are modular. One piece (monobloc) shells are either polyethylene or metal, they have their articular surface machined on the inside surface of the cup and do not rely on a locking mechanism to hold a liner in place. A monobloc polyethylene cup is cemented in place while a metal cup is held in place by a metal coating on the outside of the cup. Modular cups consist of two pieces, a shell and liner. The shell is made of metal, the outside has a porous coating while the inside contains a locking mechanism designed to accept a liner.
- Femoral Component: The femoral component is the component that fits in the femur (thigh bone). Bone is removed and the femur is shaped to accept the femoral stem with attached prosthetic femoral head (ball). There are two types of fixation: cemented and uncemented. Cemented stems use acrylicbone cement to form a mantle between the stem and to the bone. Uncemented stems use friction, shape and surface coatings to stimulate bone to remodel and bond to the implant. Stems are made of multiple materials (titanium, cobalt chromium, stainless steel, and polymer composites) and they can be monolithic or modular. Modular components consist of different head dimensions and/or modular neck orientations; these attach via a taper similar to a Morse taper. These options allow for variability in leg length, offset and version. Femoral heads are made of metal or ceramic material. Metal heads, made of cobalt chromium for hardness, are machined to size and then polished to reduce wear of the socket liner. Ceramic heads are more smooth than polished metal heads, have a lower coefficient of friction than a cobalt chrome head.
- Articular Interfaces: There are four alternative articular interfaces that could be used:
- Metal on Polyethylene: This is the traditional material which has been used for many years. There has been significant improvements in the polyethylene over the last 5 years. Ultra crossed linking of the molecules has dramatically reduced the wear of the polyethylene and this has allowed for larger ball heads to be used. With larger balled heads the risk of hip dislocation has been shown to be significantly reduced.
- Ceramic on Polyethylene: There has been significant improvements in the polyethylene over the last 5 years. Ultra crossed linking of the molecules has dramatically reduced the wear of the polyethylene. Ceramic has a very low wear rate, it is however somewhat brittle in structure and there is a small but definite incidence of fracture of the ceramic.
- Ceramic on Ceramic: This has a very low wear rate. It is also a very bioinert substance, in that the wear debris does not seem to cause significant problem either locally or elsewhere in the body. It is however somewhat brittle in structure, and there is a small but definite incidence of fracture of the ceramic. If this occurs it requires urgent revision of the articulating surfaces.
- The other baring surface is Metal on Metal which Professor Kohan does not use.Recent studies have shown that metal-on-metal devices may have problems. This is by no means universal, and there are some well functioning, well-established, durable implants which have been used and continue to be used. Metal on metal devices have been used for over 40 years in patients with high activity levels. However, some recent implants, have proved unsatisfactory, and have been withdrawn from the market.Hip resurfacing surgery at this stage can only be carried out with metal on metal implants. The metal on metal implants which are currently used have a long track record of durable, consistent, and reliable function. However, being mindful of the recent problems being attributed to metallic implants, in this practice we only use these bearings under specific circumstances, which will be discussed in detail with the patient at the time.
There are many factors that influence wear rates of implants including; patient activity levels, weight, choice of implant materials and positioning. Things that can cause the joint to fail and require further surgery would include loosening of the components which may be the result of poor bone quality, the possibility of fracture, infection, etc.These causes are difficult to predict and may occur sporadically.
Yes, this is a metallic implant, and will be detectable by metal detectors. At the airport, no documentation such as ID cards, letters, or x-rays are of help, because they are so easily forged.
Probably the best approach at the airport is patience, and a sense of humour.
Sexual relations can resume approximately four to six weeks after total hip replacement however restrictions must be kept in mind.
If you’ve have an Anterior Incision, you don’t have to be as concerned with dislocating your hip however, you should still wait approximately one month to have sex to allow your incision to heal completely.
Waiting 4-6 weeks after total hip replacement to resume sex provides several advantages:
- Your incision will be almost completely healed and less sensitive to touch
- Your hip muscles will be recovered enough to control your movements and position of your leg during sex
- Your hip will be more stable with less risk of dislocating during sexual relations
If you’ve had a Posterior Incision, precautions include:
- Avoid bending at the hip more than 90 degrees
- Avoid moving the operative leg across the midline of the body
- Avoid rotating the toes of the operative leg inward
Best Types of Positions
Missionary Position
Usually, both men and women find the missionary position most comfortable. The person with the new hip should be on the bottom. This position limits motion in the new hip, helps limit pain, and avoids expending a lot of energy. If you’re a woman, keep a slight bend in your knees with your feet on the bed. If tolerated, taking pain medication, prior to sexual relations may enhance comfort.
Face to face Position
This position can be used for either a male or female. The person with the new joint is on the bottom and can recline on pillows propped behind the back. A female can bend her knees slightly with her feet on the bed. A male can put a pillow between his knees to keep the operative leg from crossing the midline of the body.
Sitting Position
This position can be used for either a male or female. In all cases, the male sits on the chair with his knees pointing away from the midline of his body and his feet on the floor. The female sits on his lap. She must be able to have her feet planted on the floor, particularly if she has a new joint. She must avoid leaning too far forward to prevent the hip from bending more than 90 degrees.
Kneeling Position
This position can be used for either a male or female. The female with a new hip lies on her back with her buttocks near the edge of the bed. Feet must be firmly planted on the floor with knees pointing away from the midline of the body. If the male has a new hip, he can assume the position of kneeling in front of his partner. For comfort, he can use pillows under his knees. He must keep his back straight and avoid leaning over his partner to prevent the hip from bending more than 90 degrees.
Side Lying Position
This position can be used for either a male or female. In the spoon position, the person with a new hip can lie on either side. For a female with a new hip, pillows can be used to support the upper leg. A male with a new hip can drape his upper leg over his partner.
Other Side Lying Position
This position can be used for a female with a new hip. With her partner on his side, she can lie on her back and drape both legs over his body, with legs apart to keep the operative leg from crossing the midline of the body. The female can also lie on her back and drape her non-operative upper leg over her partner’s body.
Other Side Lying Positions
The partners can also face each other. The person with a new hip can lie on either side. The upper leg can be draped over the partner’s legs.
Standing Position
This position works for either a male or female. If the female has the new joint, she should lean on something firm and stay fairly upright to avoid bending the hip more than 90 degrees. If the male has the new joint, he should also avoid bending the hip more than 90 degrees.
Have a question, enquiry or referral?
Get in touch and we would be happy to help.
Phone
Locations
Bondi Junction
Suite 301C, 9 – 13 Bronte Road
Bondi Junction, NSW, 2022
