Anatomy of the Knee
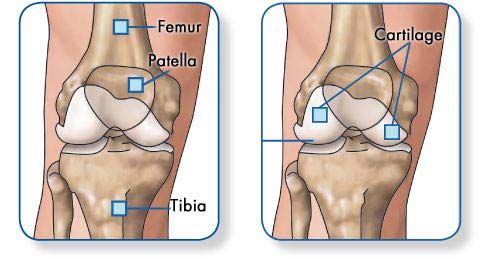
The knee is structurally complex. It is comprised of bone, ligaments, soft tissue and cartilage. Where two bones join together, it is known as a joint. The knee acts as a hinge joint. The femur or thighbone rolls across the top of the tibia or shinbone, when we walk or bend at the knee. This rolling effect produces constant but changing contact between these two bones.
Structurally the knee appears to resemble three separate joints, the correct term is compartments. The knee comprises of three compartments, medial, lateral and patello-femoral. These compartments are designed to endure the forces of every day activity. To help the knee joint cope with the constant weight bearing forces, the knee comprises of two shock absorption mechanisms.
Firstly articulating cartilage, thin smooth gristle, covers every bony surface in the joint. Secondly, two prominent pads, known as menisci or cartilages act like washers or cushions for the knee joint. Ligaments are strong strips of connective tissue like rope. A ligament provides stability for the joint.
The knee has four ligaments (medial, lateral, anterior cruciate and posterior cruciate ligaments). The knee is also stabilised by muscles. There are two major groups of muscles, the quadriceps in the front of the knee and the hamstring in the back of the knee. Soft tissue, muscle, nerves and blood vessels provide the knee with a nourishment sensation and protection. Collectively the structures work in unison to provide a well functioning joint for an individual’s lifetime.
When the knee joint has been damaged by trauma or disease the cartilage deteriorates and the bones start rubbing directly against each other (arthrosis). The result is joint pain which worsens day by day and limits motion.
Arthritis, degeneration of the bony surfaces will occur. The bony surfaces are covered with a protective skin called articulating cartilage. It is this protective coat that wears and causes raw bone to rub on raw bone. Overtime the joint slowly erodes until the underlying bone is exposed. For the individual the knee becomes painful. This can manifest as swelling, instability, limping and discomfort.
A painful knee can stop you from leading a full and happy life. Patients that exhibit moderate to severe Arthritis across the joint will benefit from knee surgery.
Start-up pain…pain when you first get up in the morning
Groin pain with walking
Knee pain with walking
Reduced range of motion & instability
A clicking sound from the knee
Redness in the knee area
Muscle Stiffness
Difficulty sleeping/night pain
A complete diagnosis of the knee can be achieved by clinical data:
Weight bearing X-ray
Patient History
Signs and Symptoms
Physical Examination
Arthroscopy
On some occasions further examination may be required.
This includes: MRI, Bone Scan and blood tests
Fractures
The most common bone broken around the knee is the patella. The ends of the femur and tibia where they meet to form the knee joint can also be fractured. Many fractures around the knee are caused by high energy trauma, such as falls from significant heights and motor vehicle collisions.
Dislocation
A dislocation occurs when the bones of the knee are out of place, either completely or partially. For example, the femur and tibia can be forced out of alignment, and the patella can also slip out of place. Dislocations can be caused by an abnormality in the structure of a person’s knee. In people who have normal knee structure, dislocations are most often caused by high energy trauma, such as falls, motor vehicle crashes, and sports-related contact.
Anterior Cruciate Ligament (ACL) Injuries
The anterior cruciate ligament is often injured during sports activities. Athletes who participate in high demand sports like soccer, football, and basketball are more likely to injure their anterior cruciate ligaments. Changing direction rapidly or landing from a jump incorrectly can tear the ACL. About half of all injuries to the anterior cruciate ligament occur along with damage to other structures in the knee, such as articular cartilage, meniscus, or other ligaments.
Collateral Ligament Injuries
Injuries to the collateral ligaments are usually caused by a force that pushes the knee sideways. These are often contact injuries. Injuries to the MCL are usually caused by a direct blow to the outside of the knee, and are often sports-related. Blows to the inside of the knee that push the knee outwards may injure the lateral collateral ligament. Lateral collateral ligament tears occur less frequently than other knee injuries.
Meniscal Tears
Sudden meniscal tears often happen during sports. Tears in the meniscus can occur when twisting, cutting, pivoting, or being tackled. Meniscal tears may also occur as a result of arthritis or aging. Just an awkward twist when getting up from a chair may be enough to cause a tear, if the menisci have weakened with age.
Tendon Tears
The quadriceps and patellar tendons can be stretched and torn. Although anyone can injure these tendons, tears are more common among middle-aged people who play running or jumping sports. Falls, direct force to the front of the knee, and landing awkwardly from a jump are common causes of knee tendon injuries.
Osteoarthritis is a progressive degenerative disease, so it has a number of different stages, and therefore a number of short and long term treatments.
Short term, osteoarthritis can be treated conservatively, by diet, exercise modification, medications and physiotherapy.
Long term, however, requires surgical intervention ranging from Arthroscopic Surgery, Knee Reconstuction & Total & Partial Knee Replacement Surgery.
If it has been determined that you require surgery to your hip Professor Kohan and his staff will give you education and guidance to help you prepare.
Various tests will be ordered depending on your medical history.
You should maintain your normal activities of daily living or regular exercise patterns to maintain movement and muscle tone.
It is also important to decrease alcohol intake and if possible, quit smoking.
Preparing your home
- Remove all rugs, loose carpets, obstacles, etc, which may be a hazard on returning home.
- Have available some extra pillows to sleep comfortably at night.
- Bathing in showering accessories may be required, such as a handheld shower.
- Provide easy access to telephone, computer, refrigerator.
- Prepare and refrigerate food before surgery, for easy access in the early postoperative period.
Hospital trip preparation
Prepare personal items to take hospital with you:
- Personal care and hygiene items
- Comfortable walking shoes
- Loose comfortable clothing
- A small amount of money
- Some reading material
- Telephone numbers of persons that may need to be contacted
- Leave valuable jewellery at home
- A list of all medications, supplements, herbs, vitamins ,etc
It is particularity important to remember to advise Professor Kohan & Dr Kerr of the various medications that you are on and then based on their medical evaluation:
Stop taking:
- 3 weeks before your surgery : Your non-steroidal anti-inflammatory (NSAID) medications such as Aspirin, Brufen, Naprosyn, Voltaren, Feldene, etc.
- 3 weeks before your surgery :Holistic and herbal medicines particularly Ginkgo and St John’s wart which may cause excessive bleeding.
Make the following appointments:
-
-
- 1 – 2 weeks prior to Surgery – Anaesthetic consult with Dr Dennis Kerr.
- 7 days post-operation – Appointment in the rooms to check the skin cut.
- 14 days post-operation – Appointment in the rooms to remove skin clips and have an ultrasound to check for a possible blood clot.
- 6 weeks post-operation – Appointment with Professor Kohan for follow-up with an X-ray.
-
Ensure the following tests have been done:
-
-
- Weight bearing X-ray.(No older than 3 months).
- Pathology (full blood count)
- Cross match Blood Test; completed a few days before surgery. This is designed to prepare blood for availability at the time of surgery.
- Chest X-ray
- ECG
-
Complete & return the following Paperwork:
-
-
- Hospital Admission Forms
- Consent Forms – signed & dated
- Estimate of Consult & Surgical Fees – signed & dated
- Estimate of Anesthetist Fees – signed & dated
- Refferal from your GP
- Ensure you have checked with your health fund about covering costs.
- Inform our office about any other health conditions. (For example, heart disease)
-
On the day of surgery:
On the day of surgery you will be expected to arrive at the hospital 2–3 hours prior to your scheduled surgery time ( if you are not admitted the night before). Call the hospital the day before your scheduled surgery date for your expected arrival time.
The operation start time is an estimate, it can be adjusted for various reasons and the staff will inform you if the time has been changed.
Once admitted, the physiotherapist will come and see you to measure you for crutches, walking frame or a cane. The physiotherapist will also provide you with education on how to use these aids.
We recommend that you wear loose fitting slacks (or shorts in the warmer weather) to the hospital. It is much easier for you after surgery. Your family is welcome to visit and stay with you prior to surgery.
When it is time for your surgery, a nurse will assist you to move to the surgical area. Once you arrive in the operating suite you will be taken to an anaesthetic bay where Dr Kerr and his anaesthetic nurse will greet you. When everything is ready, you will be taken into the operating room. The operating rooms must remain cold but extra blankets will be available for you.
- Fasting: Four hours prior to your surgery drink a glass of water. After this point do not eat or drink anything, i.e. do not eat or drink anything 4 hours prior to surgery.
- Pre-operative washing: We advise that in preparation for surgery you shower or bathe using antibacterial Phisohex emulsion. This can be used instead of soap and if used for a week or so before the operation will decrease the population of germs on the skin and by doing so, hopefully decrease the risk of infection. Phisohex can be obtained at the pharmacist and or supermarket. The day before surgery remove nail polish and makeup, if applicable.
- Your Surgical Experience: Immediately after surgery you will wake up in the recovery room. You may feel a bit groggy. Professor Kohan and his staff will monitor you, checking your blood pressure, temperature and pulse. Dr Kerr will also assess your pain level. Post-operative x-rays will be performed in recovery. After 45 minutes – 1 hour you will then be transferred back to your room on the ward.
On the day of surgery you will be expected to arrive at the hospital 2–3 hours prior to your scheduled surgery time, if you are not admitted the night before. Call the hospital the day before your scheduled surgery date for your expected arrival time.
The operation start time is an estimate, it can be adjusted for various reasons and the staff will inform you if the time is changed.
Once admitted, the physiotherapist will come and see you to measure you for crutches, walking frame or a cane if required. The physiotherapist will also provide you with education on how to use these aids.
We recommend that you wear loose fitting slacks (or shorts in the warmer weather) to the hospital. It is much easier for you after surgery. Your family is welcome to visit and stay with you prior to surgery.
When it is time for your surgery, a nurse will assist you to move to the surgical area. Once you arrive in the operating suite, you will be taken to an anaesthetic bay where Dr Kerr and his anaesthetic nurse will greet you. When everything is ready, you will be taken into the operating room. The operating rooms must remain cold but extra blankets will be available for you.
Fasting
Four hours prior to your surgery, drink a glass of water. After this point do not eat or drink anything, i.e. do not eat or drink 4 hours prior to surgery.
Pre-operative washing
We advise that in preparation for surgery, you shower or bathe using antibacterial Phisohex emulsion. This can be used instead of soap and if used for a week or so before the operation will decrease the population of germs on the skin and by doing so, hopefully decrease the risk of infection. Phisohex can be obtained at the pharmacist.
The day before surgery remove nail polish and makeup, if applicable.
Your Surgical Experience
Immediately after surgery you will wake up in the recovery room. You may feel a bit groggy. Professor Kohan and his staff will monitor you, checking your blood pressure, temperature and pulse. Dr Kerr will also assess your pain level. Post-operative x-rays will be performed in recovery.
After 45 minutes – 1 hour you will then be transferred back to your room on the ward.

Knee replacement implants are made of highly biocompatible plastic and metallic components.
The Femoral Component: This metal implant curves around the end of the femur (thighbone). It is grooved so the kneecap can move up and down smoothly against the bone as the knee bends and straightens.
The Tibial Base Plate: This is typically a flat metal platform with a cushion of strong, durable plastic, called polyethylene. Some designs do not have the metal portion and attach the polyethylene directly to the bone. For additional stability, the metal portion of the component may have a stem that inserts into the center of the tibia bone.
The Patellar component: This is a dome-shaped piece of polyethylene that duplicates the shape of the patella (kneecap), replacing the cartilage function and allowing the thigh and shin bone to slide on each other.
All components are designed so that metal always adjoins with plastic, which provides smooth movement and results in minimal wear.
There are many factors that influence wear rates of implants including; patient activity levels, weight, choice of implant materials and positioning. Things that can cause the joint to fail and require further surgery would include loosening of the components which may be the result of poor bone quality, the possibility of fracture, infection, etc.
These causes are difficult to predict and may occur sporadically.
Have a question, enquiry or referral?
Get in touch and we would be happy to help.
Phone
Locations
Bondi Junction
Suite 301C, 9 – 13 Bronte Road
Bondi Junction, NSW, 2022
